After more than a year of dealing with the ramifications of COVID-19, employers anticipate feeling the impact of the pandemic for years to come. The past 14 months have changed our interactions with and our assumptions about work. They’ve also changed what employers and employees expect of each other.
Additionally, COVID-19 has surfaced some truths about the way employers approach healthcare. Utilizing their experience and tools such as Whyzen™ Analytics from Blue Health Intelligence® (BHI®), they are implementing changes that will likely outlast the pandemic. Below are five ways COVID-19 has changed the way employers approach health benefits.
1. Mental health is as important as physical health
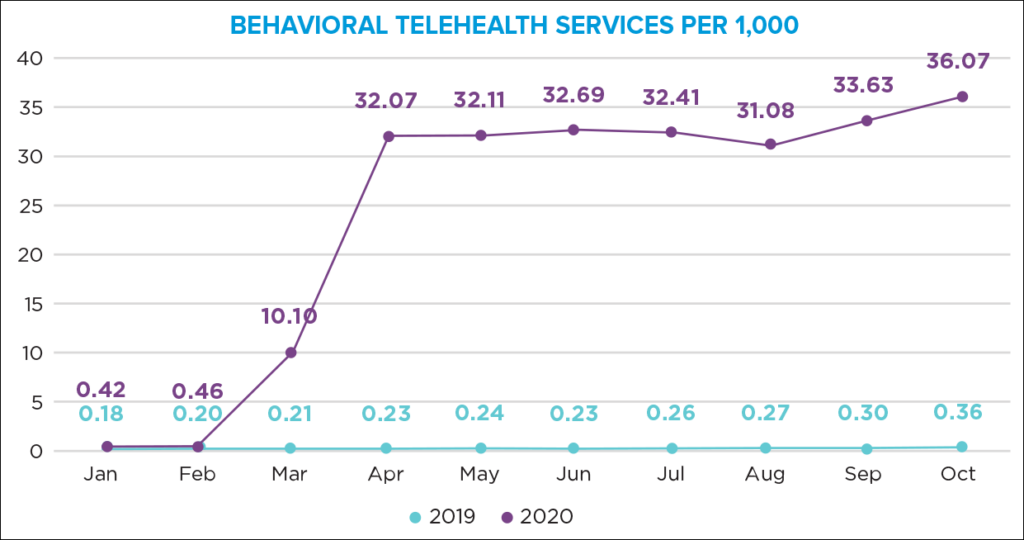
BHI data indicates that behavioral health claims spiked at the beginning of the pandemic and remained relatively constant through the end of 2020. As was true with other categories of care, patients used telehealth for their behavioral health visits. Encounters with a mental health diagnosis were more than twice as likely to take place virtually (46.1% vs 22.1%).
A survey of more than 7,700 respondents revealed that 20% experienced symptoms of anxiety during the stay-at-home orders of 2020. Pre-pandemic anxiety levels, according to the survey, were at 14%. Forty-four percent reported worse sleep quality during the lockdown and an increase in unhealthy snacking, while 27% claimed to have gained weight. Experts say these short-term impacts can have long-lasting effects.
Three out of four employers say they are increasing behavioral health benefits in 2021. And while half of benefits leaders believe their mental health stack was adequate during the pandemic, 56% of their employees with a diagnosable condition said they did not access any mental health treatment. With the renewed emphasis on mental health, employers should plan for higher utilization of mental health benefits in the months and years to come.
2. Telehealth can help employees be more productive
2020 was the year patients embraced telehealth. A study of BHI claims data by academic researchers found that, in total, one out of every seven Americans utilized telehealth to access care. In 2019, only 0.3% of ambulatory visits were billed using telehealth designations. In 2020, the rate was 24%.
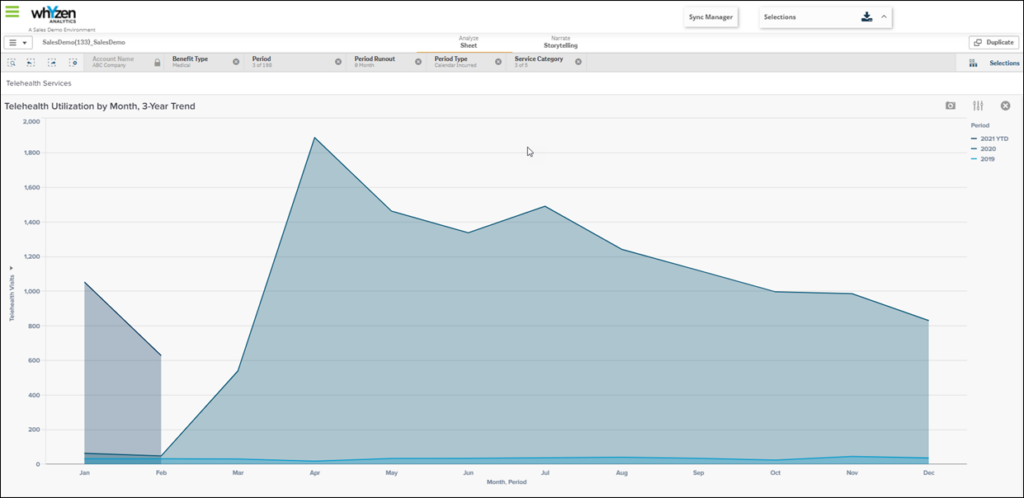
The data appears to show that telehealth will continue to be used past the pandemic. This trend could be highly beneficial for employers since telehealth may decrease absenteeism and improve productivity.
3. Employee health status needs a broader definition
When workplaces and schools shut down in response to the coronavirus, many families and neighbors couldn’t physically distance themselves. Employers began to experience the relationship between health outcomes and other social determinants of health when individuals were no longer spending eight to 12 hours a day at work.
Some employers are taking the lead in helping their employees live healthier. In central Pennsylvania, a business association is increasing employees’ access to transportation. A large employer in Alabama partnered with a wellness vendor to provide an onsite wellness program. Public policy changes can make a difference, too. A paid sick-leave ordinance adopted by the city of Austin, Texas, was shown to save employers millions by reducing turnover and increasing productivity.
Trends toward extended leave, family leave, and wellness programs indicate that employers understand their employees’ health is impacted by more than access to healthcare. Data indicate that these and other programs are investments in employee productivity and to decrease absenteeism and presenteeism.
4. Employers need novel ways to assess their employees’ well-being
COVID-19 put a spotlight on a long-standing truth in U.S. healthcare: Minorities, lower-income families, and people living in poor, urban areas are at a disadvantage when it comes to health outcomes.
In the early days of the pandemic, black and Hispanic Americans were two-and-a-half times as likely as whites to test positive for the coronavirus. In Chicago, where blacks make up about 30% of the population, more than 50% of COVID-19 cases and nearly 70% of COVID-19 fatalities were within the black population.
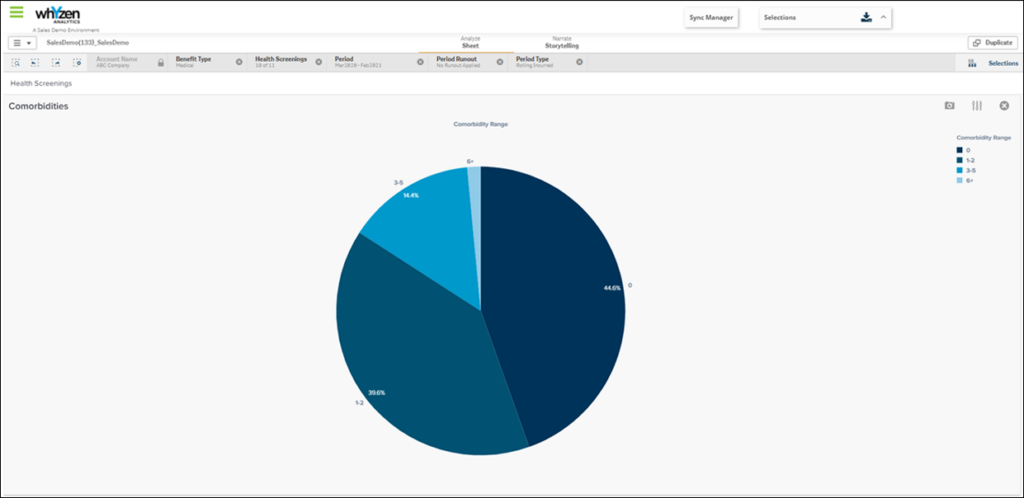
Just as a novel coronavirus made us look at different ways to approach healthcare, it can motivate us to see our employees in new ways. Demographics and life stages are a good place to start. Such segmentation can help leaders understand their employees’ needs around healthcare, childcare, retirement, transportation, and other elements. Further segmentation around mindsets and attitudes can help employers refine benefit strategies to better meet employee needs.
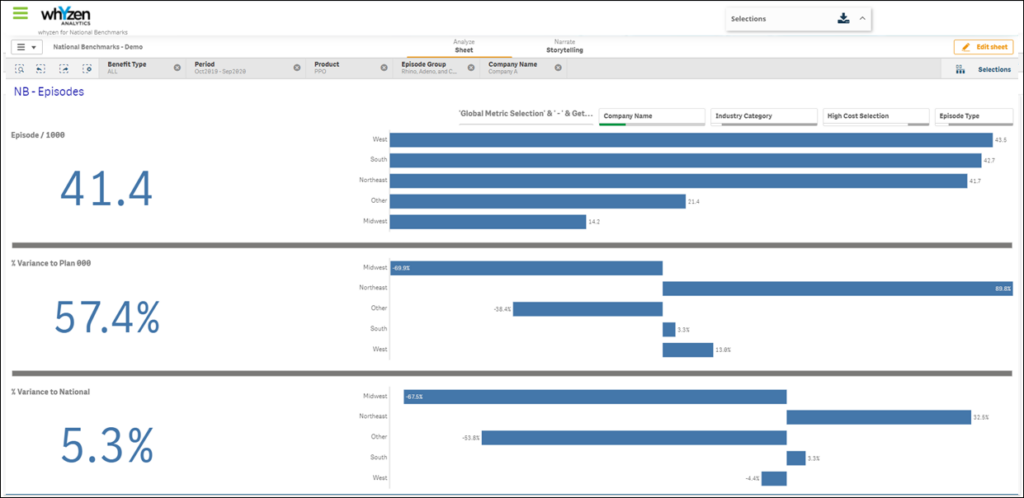
5. Access to analytics can lead to better decisions about employee health and wellness
The challenges of mental health, health access, and social determinants of health have simmered for years, but it took a pandemic for them to boil over. And in this new environment, it’s important that employers have the tools they need to make the right health benefits decisions.
- Access to up-to-date information. Staying informed about who has been newly diagnosed, hospitalized, and discharged can allow employers to be more proactive about managing employee health.
- Access to risk-adjusted intelligence. Having information adjusted by population mix and severity of illness can help employers focus resources in areas that will have the greatest impact.
- Access to benchmarking information. Benchmarking can give companies deeper insight into employee populations and health risk compared to similar employers as they work to address inequities. More sophisticated benchmarks can allow employers to make assessments on an episodic basis, which is especially important for chronic conditions.
- Access to predictive information. Predictive analytics can help employers set rates and premiums for their health benefits. This is especially true as there may be higher costs for employees who delayed care because of the pandemic.
COVID-19 has had an enduring impact on the way healthcare and health benefits are assessed and delivered. Having the data and the tools to accurately analyze that data will allow employers to help their employees be healthier, happier, and more productive.
Read more about Whyzen™ Analytics and how its predictive analytics, holistic data view, performance benchmarking, and benefit modeling helps brokers and employers design smarter benefits strategies.











